A Code Blue is a life-threatening medical emergency requiring immediate intervention, recognized across healthcare settings. This guide provides a comprehensive overview of the Code Blue procedure, detailing protocols, activation steps, roles, and best practices to ensure effective response. Its purpose is to equip healthcare professionals with the knowledge and preparedness needed to manage such critical situations efficiently, emphasizing the importance of timely and coordinated actions to save lives. Based on established guidelines and expert recommendations, this document serves as an essential resource for all staff involved in Code Blue responses.
Overview of Code Blue Procedure
A Code Blue procedure is a standardized emergency response protocol activated during life-threatening situations, such as cardiac arrest or respiratory failure. It involves immediate intervention by a trained team to provide advanced cardiac life support (ACLS). The process includes assessing the patient’s condition, initiating CPR, using defibrillators, and administering medications. Activation of Code Blue alerts the response team, ensuring prompt coordination of care. Proper use of personal protective equipment (PPE) is emphasized to safeguard responders. The goal is to restore normal heart function and stabilize the patient until further medical intervention is available. Accurate documentation of the event is critical for review and improvement.
Importance of Understanding Code Blue Protocol
Understanding the Code Blue protocol is essential for ensuring timely and effective responses to life-threatening emergencies. Proper knowledge of the procedure minimizes delays and errors, improving patient outcomes. It also ensures compliance with legal and ethical standards, reducing liability risks for healthcare providers. Clear understanding promotes efficient teamwork, enabling each team member to perform their role effectively. Additionally, it ensures proper documentation and communication, which are critical for post-event analysis and continuous improvement. Familiarity with the protocol also helps in maintaining patient privacy and confidentiality during emergencies, aligning with healthcare regulations and ethical practices.

Definition and Scope of Code Blue
Code Blue is a standardized emergency response system in healthcare settings for life-threatening situations, such as cardiac arrests, respiratory failures, or other critical conditions requiring immediate intervention by a trained response team to ensure patient safety and optimal outcomes.
What is a Code Blue?
A Code Blue is a standardized emergency response system used in healthcare settings to signal a life-threatening situation requiring immediate intervention. It is typically activated in cases of cardiac arrest, respiratory failure, or other critical medical emergencies. The term “Code Blue” is universally recognized to alert staff of the need for urgent assistance. It ensures a rapid response from a trained team, including physicians, nurses, and other healthcare professionals, to provide advanced life support and maximize the chances of a successful outcome. This system is designed to save lives by ensuring timely and coordinated action during medical crises.
Situations That Require a Code Blue Activation
A Code Blue is activated in response to life-threatening medical emergencies, such as cardiac arrest, respiratory failure, or severe trauma. It is also initiated for situations involving unresponsive patients, sudden cardiac arrhythmias, or other critical conditions requiring immediate intervention; Additionally, Code Blue may be called for acute neurological emergencies, severe allergic reactions, or any situation where a patient’s condition rapidly deteriorates. The activation ensures prompt assembly of the emergency response team to provide advanced life support and maximize the likelihood of a successful outcome. Early recognition of these situations is crucial to initiating a timely and effective response.

Code Blue Activation Process
The Code Blue process begins with identifying a life-threatening emergency, followed by immediate notification of the response team. CPR is initiated, and life-support equipment is utilized to stabilize the patient.
How to Identify a Life-Threatening Emergency
Identifying a life-threatening emergency involves recognizing signs such as loss of consciousness, absence of breathing, or no pulse. Severe injury, cardiac arrest, or respiratory failure also qualify. Staff must assess the situation quickly, ensuring immediate action is taken. The inability to breathe normally or lack of responsiveness are critical indicators. Any individual can activate a Code Blue if they witness or suspect a life-threatening condition. Timely recognition is vital to prevent further deterioration and ensure prompt intervention. Training and familiarity with emergency protocols are essential for accurate identification and swift response.
Who Can Activate a Code Blue?
Any individual can activate a Code Blue if they witness or suspect a life-threatening medical emergency. This includes healthcare staff, patients, visitors, or family members. The policy allows anyone to initiate the response to ensure timely intervention. Healthcare staff, particularly those trained in emergency procedures, are expected to take the lead. Activation involves notifying the designated response team, often through a pager system or emergency phone. Awareness of the hospital’s response zones is critical for effective coordination. Prompt action is essential, as delays can worsen patient outcomes. Training ensures that all staff understand their roles in activating and responding to a Code Blue.
Steps to Initiate a Code Blue
To initiate a Code Blue, first assess the situation to confirm a life-threatening emergency. Stay calm and quickly notify the hospital’s emergency response system, typically through a designated phone or pager. Provide clear details about the location and nature of the emergency. Ensure the area is safe and secure, and prepare for the arrival of the Code Blue team. Familiarize yourself with the equipment on hand, such as defibrillators and CPR supplies. Assign roles to team members as needed, and document the event for later review. Timely and coordinated action is critical to improving patient outcomes.
Roles and Responsibilities
Code Blue teams include first responders, nurses, and emergency physicians, each with distinct roles to ensure coordinated and effective response during life-threatening emergencies.
Code Blue Team Members and Their Roles
A Code Blue team typically includes a first responder, RN/RPN, emergency physician, and ED nurse. The first responder initiates CPR and assesses the situation. The RN/RPN manages medications and IV access, while the emergency physician oversees advanced life support. Additional roles include a defibrillator operator, chest compressor, and runners for supplies. Each member has specific duties to ensure coordinated care during emergencies. Clear communication and defined responsibilities are critical for effective response. Team members may also provide support to families or relieve others for CPR if trained, ensuring seamless operation during critical situations.
Specific Responsibilities of Each Team Member
Each Code Blue team member has distinct responsibilities. The first responder initiates CPR and operates the defibrillator. The RN/RPN administers medications, manages IV access, and documents events. The emergency physician leads the team, directs advanced life support, and makes critical decisions. Additional members may assist with CPR, act as runners for supplies, or provide support to families. Clear role definition ensures efficient coordination during emergencies, with each member focusing on their specific tasks to maximize patient outcomes and maintain order in high-stress situations.
Communication Protocols During a Code Blue
Effective communication is critical during a Code Blue. The team leader coordinates efforts, ensuring clear and concise directives. All members must communicate their actions, such as medication administration or CPR status, loudly and clearly. Designated personnel document events in real-time, while others focus on specific tasks. Communication should be direct, avoiding unnecessary discussions, to maintain focus and efficiency. The use of standardized terminology and structured updates ensures clarity and reduces errors. Proper communication protocols help maintain order and prioritize patient care during high-stress situations.
Preparation and Training
Proper preparation and training are essential for effective Code Blue responses. Regular drills, equipment familiarization, and updated protocols ensure readiness. Continuous education enhances team performance and patient outcomes.
Essential Training for Code Blue Responders
Essential training for Code Blue responders includes CPR certification, Advanced Cardiovascular Life Support (ACLS), and familiarity with defibrillator use. Regular simulation-based drills enhance teamwork and decision-making under pressure. Training also covers communication protocols, medication administration, and equipment usage. Emphasis is placed on recognizing life-threatening emergencies and initiating appropriate interventions swiftly. Periodic refresher courses ensure responders stay updated on the latest guidelines and protocols. This comprehensive training prepares healthcare professionals to act confidently and effectively during a Code Blue, improving patient outcomes and ensuring a coordinated response.
Regular Drills and Simulations
Regular Code Blue drills and simulations are crucial for maintaining preparedness and improving response efficiency. These exercises simulate real-life emergencies, allowing teams to practice coordination, communication, and decision-making. Conducted frequently, often monthly, drills help identify gaps in knowledge and procedural execution. Simulation scenarios vary to cover diverse emergencies, ensuring staff are adept at handling different situations. Post-drill debriefs enable teams to review performance, address weaknesses, and refine protocols. This iterative process ensures continuous improvement, reinforcing the importance of teamwork and timely intervention during actual Code Blue events.
Equipment Familiarization
Equipment familiarization is essential for effective Code Blue response. Healthcare staff must be proficient in using defibrillators, ventilators, suction devices, and other critical tools. Regular training sessions ensure that responders can operate equipment accurately under stress. Hands-on practice with the Code Blue cart contents, including medications and supplies, is vital. Staff should also understand the proper sequence for deploying equipment and troubleshooting common issues. Familiarization reduces delays during emergencies, ensuring swift and appropriate intervention. Regular checks and restocking of equipment are also emphasized to maintain readiness for life-threatening situations.

Code Blue Response Procedure
A Code Blue response involves immediate assessment, CPR initiation, defibrillator use, and medication administration. These actions are critical to restore cardiac function and ensure patient survival.
Initial Assessment and CPR Initiation
The initial assessment during a Code Blue involves quickly evaluating the patient’s responsiveness, breathing, and pulse. If the patient is unresponsive and not breathing or has no pulse, CPR should be initiated immediately. Proper hand placement on the chest is crucial for effective compressions. Trained responders should aim for a compression rate of 100-120 per minute, allowing the chest to fully recoil between compressions. If available, an automated external defibrillator (AED) should be used to assess the patient’s heart rhythm and deliver shocks as needed. Prompt action is critical to maintain blood circulation and oxygen delivery to vital organs, maximizing the chances of successful resuscitation. All personnel involved must wear appropriate PPE to minimize exposure risks during aerosol-generating procedures like CPR.
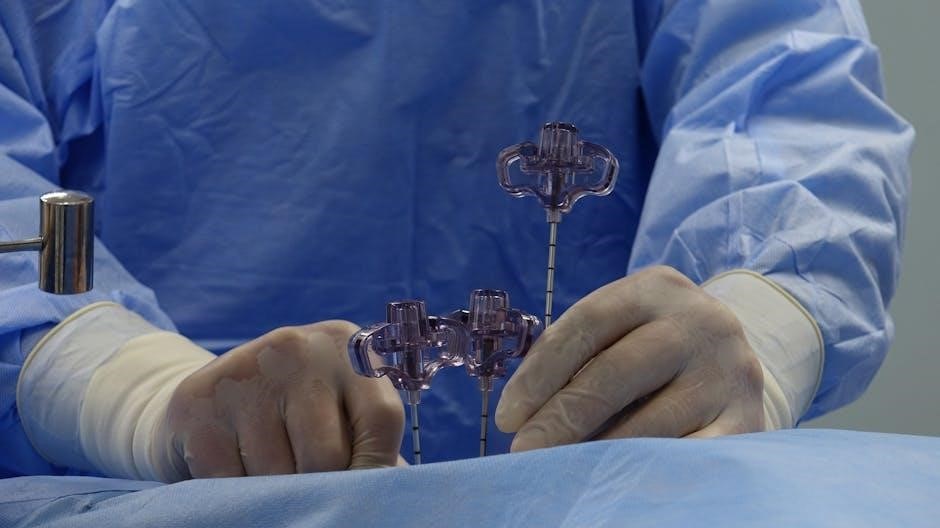
Use of Defibrillator and Other Equipment
The defibrillator is a critical tool during a Code Blue, used to restore a normal heart rhythm in cardiac arrest cases. Automated external defibrillators (AEDs) are user-friendly devices that analyze the patient’s heart rhythm and deliver shocks when necessary. Trained responders should attach the defibrillator pads to the patient’s chest, following the device’s audio prompts. Manual defibrillators, typically used in hospital settings, require a healthcare provider to interpret the heart rhythm and deliver shocks. Proper use of oxygen therapy equipment, suction devices, and IV access tools is also essential to support the patient’s airway, breathing, and circulation. All equipment must be operated by trained personnel wearing appropriate PPE to ensure safety and effectiveness during the emergency response.
Medication Administration During Code Blue
Medication administration during a Code Blue is critical for patient outcomes. Healthcare providers must administer medications as per Advanced Cardiovascular Life Support (ACLS) protocols; Common medications include epinephrine, amiodarone, and atropine, which are given to restore cardiac function. Accuracy in dosing and timing is essential to avoid complications. All medications must be documented, either on a Code Blue record or in the electronic health system. Barcode medication administration (BCMA) systems can help ensure accuracy, though exceptions may occur during emergencies. Proper labeling and verification by a second provider are recommended to maintain patient safety and adherence to protocols.
Documentation and Reporting
Accurate documentation of Code Blue events is essential for legal accountability, quality improvement, and future reference. All actions, medications, and outcomes must be recorded promptly and thoroughly.
Importance of Accurate Documentation
Accurate documentation during and after a Code Blue is critical for accountability, legal protection, and quality improvement. It ensures a clear record of events, interventions, and outcomes, aiding in post-event analysis and learning. Proper documentation also supports continuity of patient care, allowing healthcare teams to review decisions and interventions. Additionally, it helps identify trends, improve response protocols, and maintain compliance with regulatory standards. Detailed records are essential for debriefing sessions, legal reviews, and enhancing future Code Blue responses, ultimately contributing to better patient outcomes and system-wide improvements in emergency care.
What to Include in Code Blue Reports
A Code Blue report should include detailed patient information, the nature of the emergency, and the timeline of events; Document all interventions performed, such as CPR, defibrillator use, and medications administered, including dosages and times. Note the equipment used, personnel involved, and their roles. Record the patient’s vital signs and response to treatments. Include the final outcome, whether the patient was stabilized, transferred, or pronounced deceased. Also, document any post-event actions, such as debriefing sessions or equipment restocking. This comprehensive documentation ensures transparency, accountability, and improved future responses.
Review and Analysis of Code Blue Events
Reviewing and analyzing Code Blue events is crucial for improving response effectiveness. Each event should be thoroughly examined to identify strengths, weaknesses, and areas for improvement. The analysis should focus on the timing of interventions, adherence to protocols, and communication among team members. Insights gained from these reviews help refine procedures, enhance training, and ensure better patient outcomes in future emergencies. Regular debriefing sessions and feedback mechanisms further support continuous improvement, fostering a culture of learning and accountability within healthcare teams.
Post-Code Blue Procedures
Following a Code Blue, essential steps include debriefing the team, ensuring patient care continuation, and restocking equipment. Proper documentation and review of the event are critical for future improvements.
Debriefing and Team Discussion
Debriefing after a Code Blue is crucial for reviewing the response, identifying strengths, and addressing areas for improvement. The team discusses what occurred, actions taken, and decisions made. This open forum fosters collaboration and accountability, ensuring lessons learned are implemented. Documentation of the discussion is essential for continuous quality improvement. Team members share insights, and feedback is used to refine future responses. Effective communication during debriefs helps strengthen the team’s performance and preparedness for future emergencies. This process is vital for maintaining high standards of care and ensuring patient safety. It also supports the emotional well-being of the team.
Patient Care and Transfer Post-Code Blue
After a Code Blue, the patient’s care remains a top priority. The healthcare team ensures the patient is stable and monitored closely. If transfer to a higher level of care is needed, such as the ICU or CCU, it is coordinated seamlessly. The patient is accompanied by trained staff equipped to handle any complications during transport. Clear communication between teams ensures continuity of care. Documentation of the patient’s condition and treatment is maintained for legal and medical purposes. Emotional support is also provided to the patient and their family during this transition to address their concerns and anxiety effectively.
Restocking and Maintenance of Equipment
After a Code Blue, it is crucial to restock and maintain all equipment to ensure readiness for future emergencies. The Code Blue cart must be replenished with medications, supplies, and materials used during the response. Expired items should be replaced promptly, and all equipment, such as defibrillators and suction devices, must be checked for proper function. A thorough inventory is conducted to identify any missing or damaged items, which are then reordered or repaired. Regular maintenance schedules are followed to uphold the integrity of life-saving tools. This process ensures the team is always prepared to respond effectively to the next Code Blue situation.
Legal and Ethical Considerations
Code Blue responses involve legal and ethical dilemmas, requiring adherence to patient rights, privacy, and confidentiality. Proper documentation and compliance with policies are essential to mitigate liability risks.
Liability and Legal Implications
Code Blue situations raise significant legal and ethical concerns, particularly regarding patient care and responder accountability. Failure to adhere to established protocols or negligence in performing life-saving measures can result in legal liability. Healthcare providers must ensure compliance with hospital policies and standards of care to minimize risks of malpractice claims. Proper documentation of actions taken during a Code Blue is crucial, as it serves as evidence of due diligence. Additionally, violations of patient confidentiality or improper handling of sensitive information can lead to legal consequences. Understanding these implications is vital for all Code Blue responders to provide ethical and legally sound care.
Ethical Dilemmas in Code Blue Situations
Ethical dilemmas often arise during Code Blue situations, challenging responders to balance patient care with moral principles. Decisions about resuscitation, particularly for patients with Do Not Resuscitate (DNR) orders, require careful consideration. Conflicts may arise between patient autonomy and medical advice, especially in high-stress environments. Additionally, resource allocation and prioritization of care during emergencies can raise ethical concerns. These dilemmas highlight the importance of adhering to hospital policies and ethical guidelines to ensure decisions align with patient rights and medical standards. Clear communication and teamwork are essential to navigate these complex situations effectively while maintaining trust and integrity in care.
Patient Privacy and Confidentiality
Patient privacy and confidentiality are critical during Code Blue situations. While urgent care is the priority, healthcare providers must ensure patient information remains secure. All discussions and documentation related to the event should be handled discreetly, adhering to HIPAA guidelines. Access to records should be restricted to authorized personnel only. Additionally, any sharing of information with family or external parties must comply with privacy laws. Maintaining confidentiality fosters trust between patients and healthcare providers, even in life-threatening emergencies. Proper protocols for documentation and communication are essential to safeguard patient privacy while delivering timely care.

Case Studies and Real-Life Scenarios
Real-life scenarios illustrate the effectiveness of Code Blue protocols in cardiac arrests, trauma cases, and respiratory failures. These studies highlight successes, challenges, and areas for improvement, enhancing future responses.
Successful Code Blue Outcomes
Successful Code Blue outcomes often result from rapid response, effective CPR, and timely defibrillator use. Studies show improved survival rates when protocols are followed precisely. For instance, a patient experiencing cardiac arrest in a hospital setting was revived due to immediate intervention by the Code Blue team. Another case involved a trauma patient whose life was saved through swift coordination and advanced life support measures. These examples underscore the importance of training, teamwork, and adherence to established guidelines in achieving positive outcomes during life-threatening emergencies.
Lessons Learned from Code Blue Incidents
Code Blue incidents often reveal critical insights into improving response effectiveness. Common lessons include the importance of clear communication, timely equipment availability, and adherence to established protocols. For example, delays in defibrillator use or miscommunication among team members can significantly impact patient outcomes. Post-incident reviews highlight the need for regular drills and updated training to address such gaps. Additionally, accurate documentation of events is crucial for identifying trends and improving future responses. These lessons emphasize the importance of continuous improvement and preparedness in managing life-threatening emergencies effectively.
Challenges Faced During Code Blue Response
Code Blue responses often encounter challenges such as delays in activating the code, insufficiently trained staff, and equipment malfunctions. Communication breakdowns among team members can hinder coordination, while high-stress environments may lead to errors. Additionally, managing family members’ anxieties and ensuring patient privacy can complicate the situation. Timely access to necessary supplies and adhering to protocols under pressure are also common difficulties. These challenges underscore the need for regular training, efficient protocols, and clear communication to optimize response effectiveness and improve patient outcomes during critical situations.
Continuous Improvement
Continuous improvement in Code Blue response involves implementing feedback from past events, updating protocols with the latest medical advancements, and integrating new technologies to enhance efficiency and patient outcomes.
Feedback Mechanisms for Code Blue Teams
Effective feedback mechanisms are crucial for improving Code Blue responses. Post-event debriefing sessions allow team members to discuss what went well and identify areas for improvement. Standardized evaluation forms are used to document performance and suggest enhancements. Open communication channels ensure that all voices are heard, fostering a culture of continuous learning. Regular reviews of feedback help refine protocols, update training materials, and address systemic issues. By prioritizing feedback, Code Blue teams can evolve and deliver higher-quality care in future emergencies.
Updates in Code Blue Protocols
Code Blue protocols are continually updated to reflect advances in medical knowledge and technology. Recent updates emphasize the importance of early defibrillation and high-quality CPR to improve survival rates. Guidelines now incorporate the use of automated external defibrillators (AEDs) and advanced airway management techniques. Additionally, updated protocols prioritize the use of personal protective equipment (PPE) during aerosol-generating procedures to safeguard rescuers. Regular reviews of evidence-based practices ensure that Code Blue responses remain aligned with the latest standards of care, enhancing patient outcomes and team safety.
Technology Advancements in Code Blue Response
Advancements in technology have significantly enhanced Code Blue responses, improving efficiency and patient outcomes. Automated external defibrillators (AEDs) now include real-time guidance and data transmission to healthcare teams. Smart hospital systems enable rapid alerting and coordination of responders through mobile devices. AI-driven algorithms analyze vital signs, predicting cardiac arrests earlier. Additionally, telemedicine integration allows remote experts to assist during emergencies. Digital documentation tools streamline post-event reporting and analysis, ensuring better preparedness for future incidents. These innovations collectively improve response times, communication, and the quality of care provided during life-threatening situations.
Effective Code Blue management is critical for patient survival, emphasizing timely intervention, clear communication, and adherence to established protocols. Understanding these procedures is vital for all healthcare professionals.
A Code Blue procedure is a structured response to life-threatening medical emergencies, requiring immediate action and coordination among healthcare teams. Key components include rapid identification of emergencies, proper activation protocols, and the roles of responders. Effective communication, use of equipment like defibrillators, and adherence to ACLS guidelines are critical. Documentation and debriefing post-event ensure continuous improvement. Training, regular drills, and equipment maintenance are essential for preparedness. Understanding these elements ensures a unified and efficient response, ultimately improving patient outcomes and safety in healthcare settings. This guide provides a clear framework for managing Code Blue situations effectively.
Final Thoughts on Effective Code Blue Management
Effective Code Blue management hinges on preparation, clear communication, and seamless teamwork. Ensuring all staff are trained and familiar with protocols is crucial. Regular drills and debriefing sessions help identify areas for improvement, fostering a culture of continuous learning. Adherence to established guidelines, proper use of equipment, and timely documentation are essential for optimal outcomes. By staying updated on best practices and maintaining a proactive approach, healthcare teams can enhance their response to life-threatening emergencies, ultimately saving lives and improving patient care. A well-coordinated Code Blue response reflects a commitment to excellence in healthcare.

